Testing irreplaceable body fluids
When body fluid tests are ordered, we typically think of blood, saliva and urine. Although these body fluids are commonly tested for assessing health, they are not the only body fluids that can be tested to find what ails you. Other routinely tested body fluids include cerebrospinal fluid (CSF), serous fluids (pleural, peritoneal and pericardial) and synovial fluid. Each fluid type has a unique composition and generally is considered an irreplaceable specimen since collection is often invasive.
5 irreplaceable body fluids:
1. Cerebrospinal fluid
What is it?
Cerebrospinal fluid (CSF) is the liquid around your brain and spinal cord. This fluid helps protect the brain and spinal cord from injury. It also helps remove waste products, antibodies, chemicals and foreign substances from the brain and spinal cord. Cerebrospinal fluid is made up of approximately 99% water and a group of cells called choroid plexus. Your body has about 150 milliliters of fluid ‒ roughly two-thirds of a cup.
Your body has about 150 mL – roughly two-thirds of a cup – of cerebrospinal fluid.
What is it being tested for?
Cerebrospinal fluid should be clear and colorless. If the cerebrospinal fluid appears cloudy or is not clear, it may be an indication of many disorders or diseases. The clinicians will examine cerebrospinal fluid for a presence of red blood cells, white blood cells, bacteria or high levels of proteins. The goal is to rule out infectious diseases of the brain and spinal cord such as meningitis and encephalitis, autoimmune disorders such as multiple sclerosis, bleeding of the brain and brain tumors.
2. Synovial fluid
What is it?
Synovial fluid is found in your joints (elbow, knee, hip, shoulder, wrist, etc.) and is a natural lubricant that cushions the bones so they won’t rub together. This body fluid can be straw colored or clear and can be moderately sticky. Synovial fluid can form strings a few inches long.
What is it being tested for?
Synovial fluid is examined for changes in the appearance and physical characteristics when trying to uncover the causes of inflammation, pain, swelling and fluid accumulation in the joints. If the fluid has become cloudy, it may indicate the presence of microbes, white blood cells or crystals. If the synovial fluid is reddish in color, there may be a presence of red blood cells. Synovial fluid is often tested using chemical tests or microscopic examination. The clinicians look at synovial fluid for diagnosing acute and/or chronic arthritis, bleeding disorders such as hemophilia, inflammatory diseases such as gout and pseudogout, rheumatoid arthritis, lupus or degenerative diseases such as osteoarthritis. Gout and pseudogout are diagnosed by the crystals that are formed in the joint, such as uric acid crystals (gout) and calcium pyrophosphate dihydrate crystals (CPPD for pseudogout) which typically affect the feet and legs.
Gout and pseudogout are diagnosed by the presence of crystals in the synovial fluid.
3. Pleural fluid
What is it?
Pleural fluid is a thin translucent fluid (contains white blood cells) that fills the cavity between the parietal (outer) and visceral (inner) pleural layers surrounding the lungs, which acts as a lubricant and helps facilitate breathing. In a healthy person the volume of fluid is small, roughly 10 mL to 20 mL. This body fluid helps maintain a negative pressure between lungs and thoracic cavity to keep lungs properly inflated for normal breathing.
What is it being tested for?
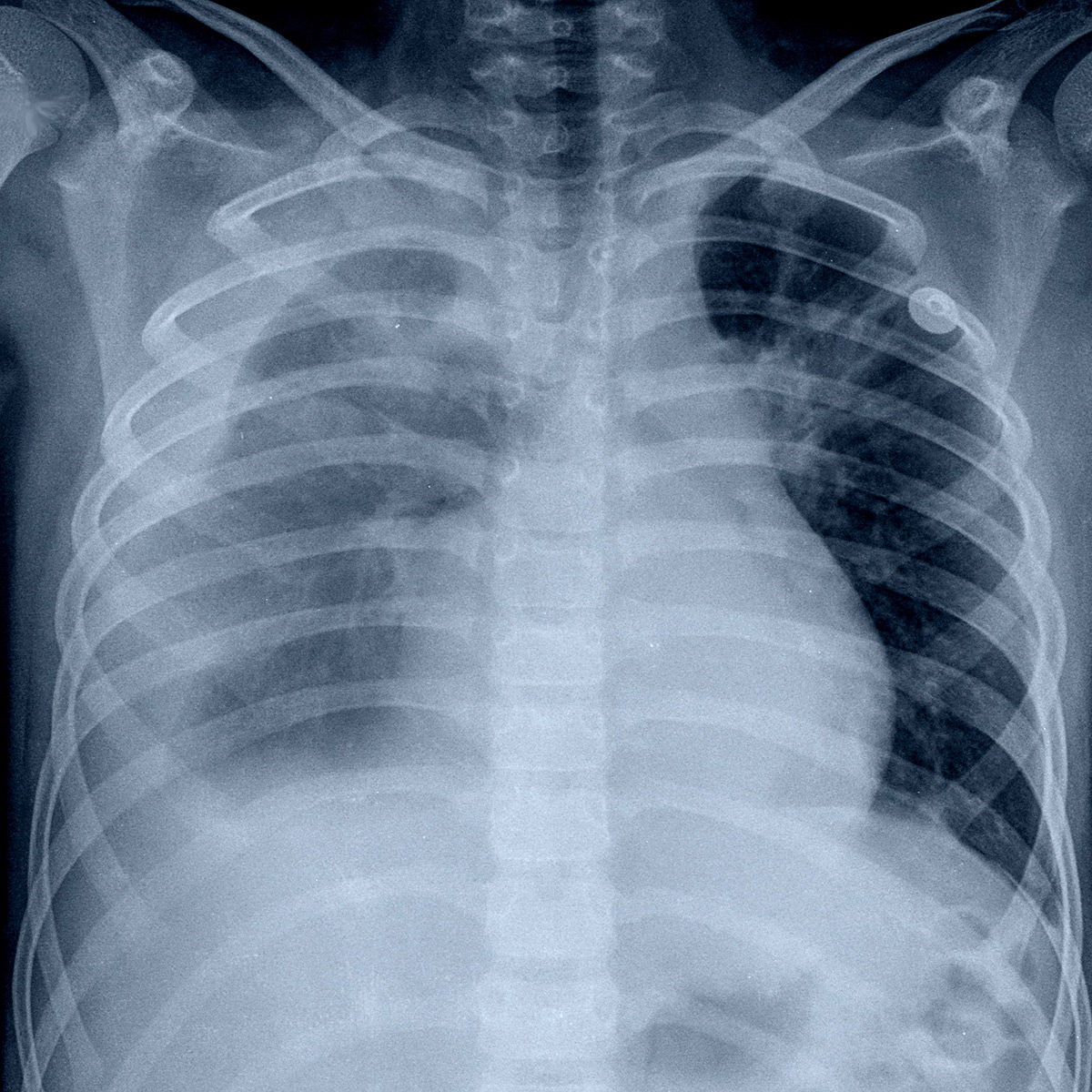
New pleural fluid is continually put in circulation while it is also being continually reabsorbed into the lymphatic system. Changes in the volume of pleural fluid can be caused by infection, trauma or other causes and can lead to respiratory problems and other adverse conditions. Extraction of pleural fluid allows doctors to diagnose causes of these changes or to investigate for signs of infection or disease. An excessive accumulation of pleural fluid in the chest cavity, which can cause shortness of breath or a collapse in the lung, is called pleural effusion. There are many causes for pleural effusion, including heart failure, pulmonary embolism, cirrhosis, pneumonia, cancer, kidney disease, inflammatory disease and autoimmune disease.
4. Pericardial fluid
What is it?
Pericardial fluid surrounds your heart in the pericardial cavity contained in the pericardial sac. This body fluid lubricates the two layers of the serous membrane, helping them glide over each other with every heartbeat.
What is it being tested for?
Pericardial effusion is the increase in the amount of pericardial fluid that surrounds the heart. When analyzing the pericardial fluid, it is important to determine if the increase in fluid is due to an imbalance of the pressure in blood vessels (transudate) or an injury or inflammation of the pericardium (exudate). The set of tests run to determine transudate or exudate includes cell count, protein or albumin levels, and appearance of the fluid. Once this is determined, the cause for the buildup of fluid can be traced to conditions including congestive heart failure, cirrhosis, infection, cancer malignances or an autoimmune disease.
5. Peritoneal fluid
What is it?
Peritoneal fluid is a liquid made in the abdominal cavity which lubricates the surface of tissue that lines the abdominal wall and pelvic cavity. It covers most of the organs in the abdomen. There is approximately 5 mL to 20 mL of fluid between the layers of the peritoneum that lines the abdominal wall.
What is it being tested for?
When an increased amount of peritoneal fluid is found in the body’s cavity it is sent to the lab to be tested for albumin, protein, red blood cells, white blood cells, bacteria and other infections. An increased volume of peritoneal fluid is called ascites. Ascites can be caused by cirrhosis of the liver, cancer, congestive heart failure, tuberculosis, malignances, autoimmune disease or other conditions.
“Manual body fluid analysis can be time consuming and has a high degree of technologist-to-technologist variability.”
Manual body fluid analysis can be time consuming and has a high degree of technologist-to-technologist variability. Today’s hematology instruments are equipped with advanced technologies that provide improved efficiency, precision and accuracy. Automating body fluid analysis will decrease turnaround times for most body fluid samples by eliminating the need for duplicate manual hemacytometer testing and reduce intralaboratory variability.
Streck’s Cell-Chex® Auto is the first automated body fluid count control for Abbott®, Beckman Coulter®, Siemens Healthcare Diagnostics and Sysmex® hematology instruments.
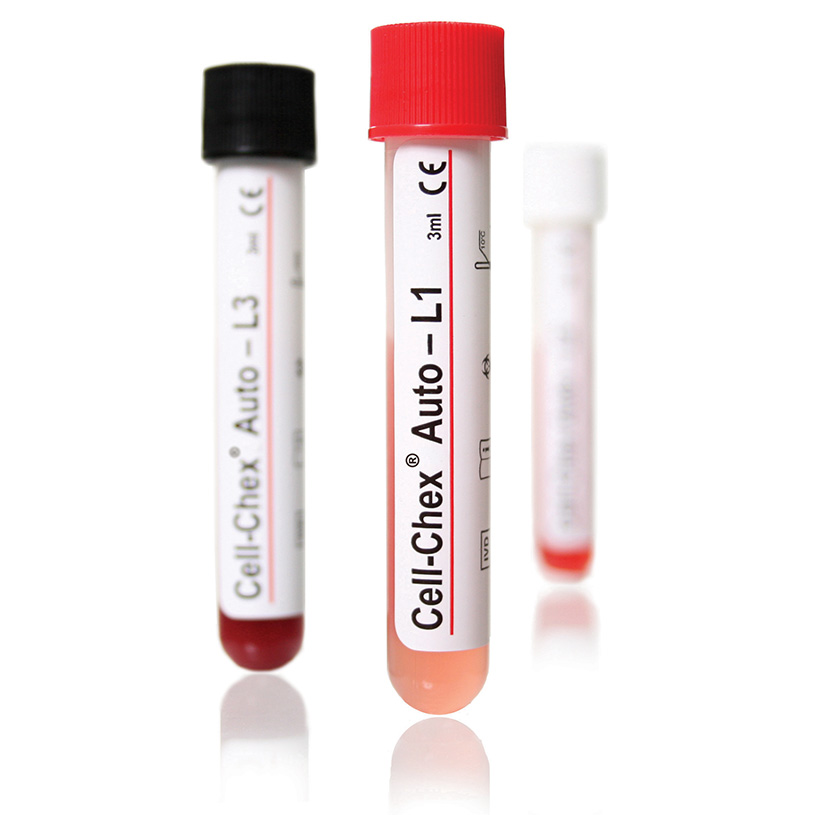
Streck’s Cell-Chex® is an assayed control intended for monitoring total cell counts performed manually using a hemacytometer to validate quantitation of red and white blood cells in patient cerebrospinal fluid and body fluid samples including pleural, pericardial, peritoneal and synovial fluid. Level 1-UC contains monosodium urate crystals, and Level 1-CC contains Calcium Pyrophosphate Dihydrate (CPPD) crystals, which can be used to monitor the presence of crystals in synovial fluid. The white blood cells in Cell-Chex are human cells to better resemble patient samples. When stained in the same manner as a patient sample, the technologist can differentiate granulocyte, lymphocyte and monocyte populations.
Click here for more information about our body fluid controls.


CLIA Announces New 2024 Updates